Integumentary System Medical Terminology: An Overview
Understanding the language of the integumentary system—skin, hair, and nails—is crucial for healthcare professionals; this overview provides a foundational understanding of related terminology.
This system provides overall body protection, and its study involves analyzing, defining, and building medical terms related to its structure and function.
Key components include derm/o, cutane/o, epiderm/o, melan/o, and understanding prefixes like hyper- and hypo- alongside suffixes such as -itis and -ectomy.
The integumentary system, encompassing the skin and its accessory structures – hair, nails, and glands – represents the body’s first line of defense against the external environment. It’s a dynamic, multifaceted system responsible for crucial functions beyond simple protection, including temperature regulation, sensation, vitamin D synthesis, and immune response.
Understanding the medical terminology associated with this system is paramount for effective communication within healthcare. This system’s largest organ, the skin, can weigh over 20 pounds in adults, highlighting its significant role. Studying its components requires familiarity with root words, prefixes, and suffixes, enabling accurate interpretation of medical records and diagnoses.
This introduction serves as a gateway to deciphering the language used to describe conditions, procedures, and anatomical features related to the skin. Analyzing terms allows for a deeper comprehension of dermatological health and disease, facilitating informed patient care and research.
Components of the Integumentary System
The integumentary system is comprised of several key components working in concert to maintain bodily health. Primarily, it includes the skin itself – the cutaneous membrane – which is structured in layers of cells and tissues supported by connective tissue. Accessory structures, vital to the system’s function, are hair follicles, sebaceous glands, and sweat glands.
Skin, as the largest organ, provides a protective barrier. Hair offers insulation and sensory input, while nails protect the distal phalanges. Sebaceous glands secrete sebum, lubricating the skin and hair, and sweat glands regulate temperature through perspiration. These components are interconnected and contribute to the system’s overall integrity.
Understanding the terminology related to each component is essential. Terms describing skin layers, gland types, and hair structures form the basis of dermatological communication. Accurate identification and description of these components are crucial for diagnosis and treatment.

Key Root Words & Combining Forms
Mastering root words like derm/o, cutane/o, epiderm/o, and melan/o unlocks the ability to decipher and construct complex integumentary system medical terminology effectively.
Derm/o & Cutane/o – Relating to Skin
Both “derm/o” and “cutane/o” are fundamental combining forms signifying “skin.” “Derm/o” originates from the Greek word “derma,” meaning skin, and is widely used in medical terminology to denote structures or conditions pertaining to the skin itself.

Similarly, “cutane/o” stems from the Latin “cutis,” also translating to skin. These roots appear in numerous terms describing skin-related ailments, procedures, and anatomical features.
For instance, “dermatitis” (inflammation of the skin) utilizes “derm/o,” while “subcutaneous” (under the skin) employs “cutane/o.” Recognizing these roots is essential for breaking down and understanding complex medical terms related to dermatology and the integumentary system as a whole. Understanding these roots facilitates accurate interpretation and communication within the healthcare field.
Epiderm/o – Relating to the Epidermis
The combining form “epiderm/o” specifically refers to the epidermis, the outermost layer of skin. Derived from the Greek “epi” (upon) and “derma” (skin), it denotes structures or conditions situated upon the skin, or relating directly to this vital protective layer.
The epidermis is responsible for shielding underlying tissues from environmental hazards, and “epiderm/o” appears in terms describing conditions affecting this layer, such as “epidermolysis” (dissolution of the epidermis).
Understanding this root is crucial because the epidermis is frequently involved in various dermatological conditions. Recognizing “epiderm/o” allows for a precise understanding of the location and nature of skin-related pathologies; Furthermore, it aids in deciphering medical reports and communicating effectively about epidermal health and treatments within a clinical setting.
Hypoderm/o – Relating to the Subcutaneous Layer
The combining form “hypoderm/o” denotes the subcutaneous layer, also known as the hypodermis, situated below the dermis. “Hypo” signifies below, and “derm/o” relates to skin, accurately describing its anatomical position. This layer is primarily composed of adipose (fat) tissue and connective tissue.
The hypodermis serves as an insulator, cushions underlying structures, and provides a reserve of energy. Terms utilizing “hypoderm/o” often describe conditions affecting this layer, such as “hypodermic” (injected into the subcutaneous tissue).
Comprehending this root is vital as the hypodermis plays a significant role in temperature regulation and shock absorption. Accurate interpretation of medical terminology involving “hypoderm/o” is essential for understanding diagnoses and treatment plans related to this deeper skin layer. Therefore, it’s a key component of integumentary system knowledge.
Melan/o – Relating to Pigment
The combining form “melan/o” directly relates to pigment, specifically melanin, responsible for skin, hair, and eye color. Derived from the Greek word “melas” meaning black, it signifies the presence or absence of pigmentation. Melanocytes, the cells producing melanin, are crucial in protecting skin from UV radiation.
Terms incorporating “melan/o” frequently describe conditions involving pigment alterations. For example, “melanoma” denotes a tumor of melanocytes, a serious form of skin cancer. “Melanocyte-stimulating hormone” (MSH) influences melanin production.
Understanding “melan/o” is essential for interpreting diagnoses related to pigmentation disorders, such as albinism (lack of melanin) or hyperpigmentation (excess melanin). Accurate terminology comprehension aids in recognizing potential risks and appropriate medical interventions. Consequently, it’s a fundamental element within integumentary system terminology.

Common Prefixes
Prefixes significantly modify integumentary term meanings; “hyper-” indicates excessive conditions, while “hypo-” denotes deficiency. “Erythr/o” signifies redness, aiding precise description.
Hyper- – Excessive
The prefix “hyper-”, originating from Greek, fundamentally alters a term’s meaning to denote excess or above normal levels. Within the context of the integumentary system, this prefix is frequently encountered when describing conditions characterized by heightened activity or overproduction.
For instance, hyperhidrosis signifies excessive sweating, a condition where the sweat glands are overactive, leading to noticeable perspiration beyond what’s typical for thermoregulation or emotional responses. Similarly, hyperkeratosis describes a thickening of the stratum corneum, the outermost layer of the epidermis, resulting in scaly or rough skin patches.
Understanding “hyper-” is crucial for accurately interpreting medical documentation and diagnoses related to skin disorders. It signals an amplification of a normal process, often indicating an imbalance requiring medical intervention to restore homeostasis and alleviate associated symptoms.
Hypo- – Deficient
The prefix “hypo-”, derived from Greek, indicates a deficiency, reduction, or below-normal level. In integumentary terminology, it signals a lack or decreased function related to skin, hair, or associated structures. Recognizing this prefix is vital for accurate medical interpretation.
Hypopigmentation, for example, describes a loss of pigment in the skin, resulting in lighter patches compared to surrounding areas. This contrasts with hyperpigmentation, indicating excess pigment. Hypodermic, while relating to the subcutaneous layer, can imply a deficiency in fat or tissue within that layer.
Hypoalgesia refers to a diminished sensitivity to pain, potentially impacting a patient’s ability to detect skin injuries. Comprehending “hypo-” allows healthcare professionals to quickly identify conditions characterized by reduced function or substance levels within the integumentary system, guiding appropriate diagnostic and therapeutic approaches.
Erythr/o – Redness
The combining form “erythr/o”, stemming from the Greek word for “red,” denotes redness or a red coloration. Within integumentary medical terminology, it frequently indicates inflammation, increased blood flow, or conditions affecting skin coloration. Recognizing this root is crucial for deciphering various dermatological terms.
Erythema, a common term, specifically refers to redness of the skin, often caused by inflammation or capillary dilation. Erythrodermia signifies widespread redness and scaling of the skin, indicating a more severe inflammatory process. Understanding “erythr/o” aids in identifying conditions involving visible redness.
Furthermore, it appears in terms describing specific skin conditions presenting with redness, such as erythematous rashes. Healthcare professionals utilize this knowledge to quickly assess and diagnose skin abnormalities, linking the observed redness to underlying pathological processes within the integumentary system.

Suffixes Used in Integumentary Terminology
Suffixes significantly alter a root word’s meaning, denoting conditions like inflammation (-itis), tumors (-oma), surgical removal (-ectomy), and disease (-pathy).
-itis – Inflammation
The suffix -itis universally denotes inflammation, a protective response characterized by redness, swelling, heat, and pain, within a specific body part or system.
In integumentary terminology, combining -itis with a root word creates terms describing inflammatory skin conditions.
Dermatitis, for example, signifies inflammation of the skin, encompassing various causes like eczema or allergic reactions.
Similarly, folliculitis indicates inflammation of the hair follicles, often presenting as small, red bumps.
Understanding -itis is fundamental because inflammation is a common symptom and diagnostic indicator in numerous dermatological presentations.
Recognizing this suffix allows for quick interpretation of medical terms and a clearer understanding of the underlying pathological process affecting the integumentary system.
It’s a cornerstone for accurate communication and documentation within healthcare settings.
-oma – Tumor
The suffix -oma signifies a tumor, which can be benign or malignant, representing an abnormal mass of tissue growth.
Within the integumentary system, -oma is crucial for defining various skin growths and neoplasms.
Melanoma, a particularly serious condition, denotes a tumor originating from melanocytes, the pigment-producing cells, often presenting as a dark, irregularly shaped mole.
Lipoma, conversely, represents a benign tumor composed of fatty tissue, typically soft and movable under the skin.
Fibroma indicates a benign tumor of fibrous connective tissue.
Understanding -oma is vital for accurate diagnosis and treatment planning, as the nature of the tumor—benign versus malignant—significantly impacts the prognosis and therapeutic approach.
It’s a key component in dermatological terminology, enabling precise communication about skin lesions and growths.
-ectomy – Surgical Removal
The suffix -ectomy denotes the surgical removal of a part or the entirety of a structure.
In the context of the integumentary system, this commonly refers to the excision of skin lesions, tumors, or affected tissues.
Biopsy, while involving removal, is often a diagnostic procedure, but larger excisions fall under -ectomy.
Nevus-ectomy signifies the surgical removal of a nevus, commonly known as a mole, often performed when it exhibits suspicious characteristics.
Tumor-ectomy indicates the removal of a tumorous growth from the skin.
Understanding -ectomy is crucial for comprehending surgical procedures related to skin conditions;
The procedure’s extent and location are often specified with a prefix indicating the structure being removed, ensuring precise medical documentation and communication.
-plasty – Surgical Repair
The suffix -plasty signifies a surgical procedure focused on repairing or reconstructing a damaged or defective body part.
Within the integumentary system, this often involves restoring skin integrity or improving its aesthetic appearance.
Derm-plasty, commonly known as a skin graft, involves transplanting skin tissue to cover wounds or burns, facilitating healing and minimizing scarring.
Rhino-plasty, while primarily associated with the nose, can include skin repair and reshaping of facial structures.
Understanding -plasty requires recognizing that it’s not simply removal, but a reconstructive process.
Cosmetic procedures, like facelifts, also fall under this category, aiming to improve skin tone and reduce wrinkles.
The term clearly indicates a restorative surgical intervention, crucial for accurate medical terminology comprehension.
-graphy – Recording
The suffix -graphy denotes the process of visually recording or creating an image of a body part or function.
In the context of the integumentary system, this primarily relates to documenting skin conditions and structures.
Derm-graphy, encompassing techniques like photography and dermatoscopy, allows for detailed visualization of skin lesions, moles, and other abnormalities.
These recordings are essential for monitoring changes over time and aiding in accurate diagnoses.
Furthermore, specialized imaging techniques, such as thermal imaging, can record temperature variations on the skin surface, indicating inflammation or vascular issues.
The resulting images serve as valuable documentation for patient records and communication among healthcare professionals.
-graphy emphasizes the visual aspect of assessment, providing a permanent record for analysis and treatment planning.
-pathy – Disease
The suffix -pathy signifies disease or abnormal condition, indicating a deviation from normal health within a specific body part or system.
When applied to the integumentary system, -pathy forms terms describing various skin diseases and disorders.
Dermat-pathy, for instance, broadly refers to any disease affecting the skin, encompassing a wide range of conditions from mild rashes to severe infections.
Specific examples include neurodermatopathy, a chronic inflammatory skin condition, and chromhidrosis, a disorder affecting sweat gland function.
Understanding this suffix is crucial for interpreting medical diagnoses and treatment plans related to skin ailments.
-pathy highlights the pathological aspect of a condition, emphasizing the presence of disease rather than simply inflammation or structural changes.
It’s a fundamental component in constructing and deciphering integumentary medical terminology.
Specific Integumentary Medical Terms
Key terms like dermatitis—skin inflammation—and melanoma—a tumor of melanocytes—illustrate how root words, prefixes, and suffixes combine to define specific conditions.
Biopsies, involving tissue removal, are diagnostic procedures crucial for accurate diagnoses within the integumentary system.
Dermatitis – Inflammation of the Skin
Dermatitis, clinically defined as inflammation of the skin, encompasses a broad spectrum of conditions, each presenting with unique characteristics and underlying causes.
The term itself breaks down: “derm/o” signifying skin, and “-itis” denoting inflammation, clearly indicating the affected tissue and pathological process.
Various types exist, including atopic dermatitis (eczema), contact dermatitis (caused by irritants or allergens), and seborrheic dermatitis (affecting oily areas).
Symptoms commonly include redness, itching, swelling, blistering, and scaling, significantly impacting a patient’s quality of life.
Diagnosis often involves a physical examination, patient history, and sometimes skin biopsies to identify the specific type and triggers.
Treatment strategies range from topical corticosteroids and emollients to systemic medications and allergen avoidance, tailored to the individual case.
Understanding the nuances of dermatitis is vital for accurate diagnosis and effective management within the integumentary system.
Melanoma – Tumor of Melanocytes
Melanoma represents a serious and potentially life-threatening form of skin cancer originating in melanocytes, the cells responsible for producing melanin—skin pigment.
The term’s etymology reveals its nature: “melan/o” relating to pigment, and “-oma” indicating a tumor or growth, pinpointing the affected cells and abnormality.
Unlike other skin cancers, melanoma has a higher propensity to metastasize, spreading to distant sites within the body if left untreated.
Risk factors include excessive ultraviolet (UV) radiation exposure, fair skin, a family history of melanoma, and numerous or atypical moles.
Early detection is crucial, often utilizing the “ABCDE” rule (Asymmetry, Border irregularity, Color variation, Diameter, and Evolving).
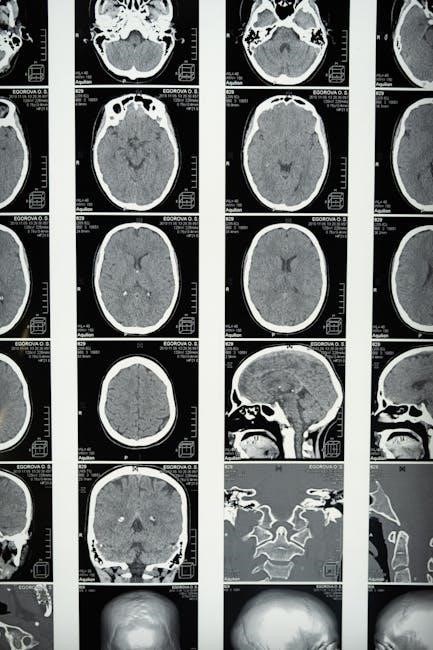
Diagnosis typically involves a skin biopsy followed by staging to determine the extent of the cancer’s spread.
Treatment options include surgical excision, immunotherapy, targeted therapy, and radiation, depending on the stage and characteristics of the melanoma.
Biopsy – Removal of Tissue for Examination
A biopsy is a crucial diagnostic procedure involving the removal of a small tissue sample from the body for microscopic examination by a pathologist.
Within the context of the integumentary system, skin biopsies are frequently performed to diagnose skin conditions, including cancers, inflammatory diseases, and infections.
The procedure typically involves local anesthesia to minimize discomfort, followed by the removal of a tissue sample using various techniques like shave, punch, or excisional biopsy.
The choice of technique depends on the size, location, and suspected nature of the lesion.
The extracted tissue is then processed, sectioned, and stained to allow the pathologist to visualize cellular structures and identify any abnormalities.
Biopsy results provide essential information for accurate diagnosis and guide appropriate treatment decisions;
It is a cornerstone of dermatological practice, enabling precise identification of skin pathologies and improving patient outcomes.

Abbreviations & Acronyms
Common abbreviations like Tx (treatment) and Dx (diagnosis) streamline communication within medical documentation regarding integumentary conditions and patient care plans.
Tx – Treatment
Within the realm of integumentary medicine, “Tx” universally signifies “treatment,” representing the interventions employed to manage and resolve skin conditions, disorders, and injuries.
Treatment modalities are incredibly diverse, ranging from topical applications – creams, ointments, and lotions – designed to address localized issues like dermatitis or fungal infections, to systemic medications administered orally or intravenously for more widespread or severe conditions.
Surgical procedures, including excisions for melanoma or reconstructive plastic surgery following trauma, also fall under the umbrella of “Tx.”
Furthermore, “Tx” encompasses non-invasive therapies such as phototherapy (light therapy) for psoriasis, cryotherapy (freezing) for warts, and various dermatological dressings to promote wound healing.
Accurate documentation of the “Tx” plan, including specific medications, dosages, frequency, and duration, is paramount for effective patient care and continuity of treatment.
The abbreviation ensures concise and efficient communication among healthcare professionals involved in the patient’s integumentary health journey.
Dx – Diagnosis
In the context of the integumentary system, “Dx” is a widely recognized abbreviation for “diagnosis,” representing the identification of a skin condition or disease through careful evaluation and testing.
The diagnostic process often begins with a thorough patient history, encompassing symptoms, onset, duration, and any relevant medical background.
A comprehensive physical examination of the skin, hair, and nails follows, noting any visible abnormalities like rashes, lesions, or changes in pigmentation.
Diagnostic procedures may include skin biopsies – removing tissue samples for microscopic analysis – to confirm suspected conditions like melanoma or psoriasis.
Further testing, such as patch testing for allergies or fungal cultures to identify infections, can refine the “Dx.”
Precise “Dx” is crucial for guiding appropriate treatment plans and ensuring optimal patient outcomes within dermatological care.
